Drug detox is the initial step in overcoming substance dependence, focusing on the safe removal of toxic substances from the body. It is a medically supervised process designed to manage withdrawal symptoms and help individuals achieve physical stability before continuing treatment. According to the 2020 National Survey of Substance Abuse Treatment Services (N-SSATS), there were 1,839 facilities in the United States providing detoxification services. Detox is essential for those struggling with addiction, as attempting to quit abruptly without medical support is dangerous and, in some cases, life-threatening.
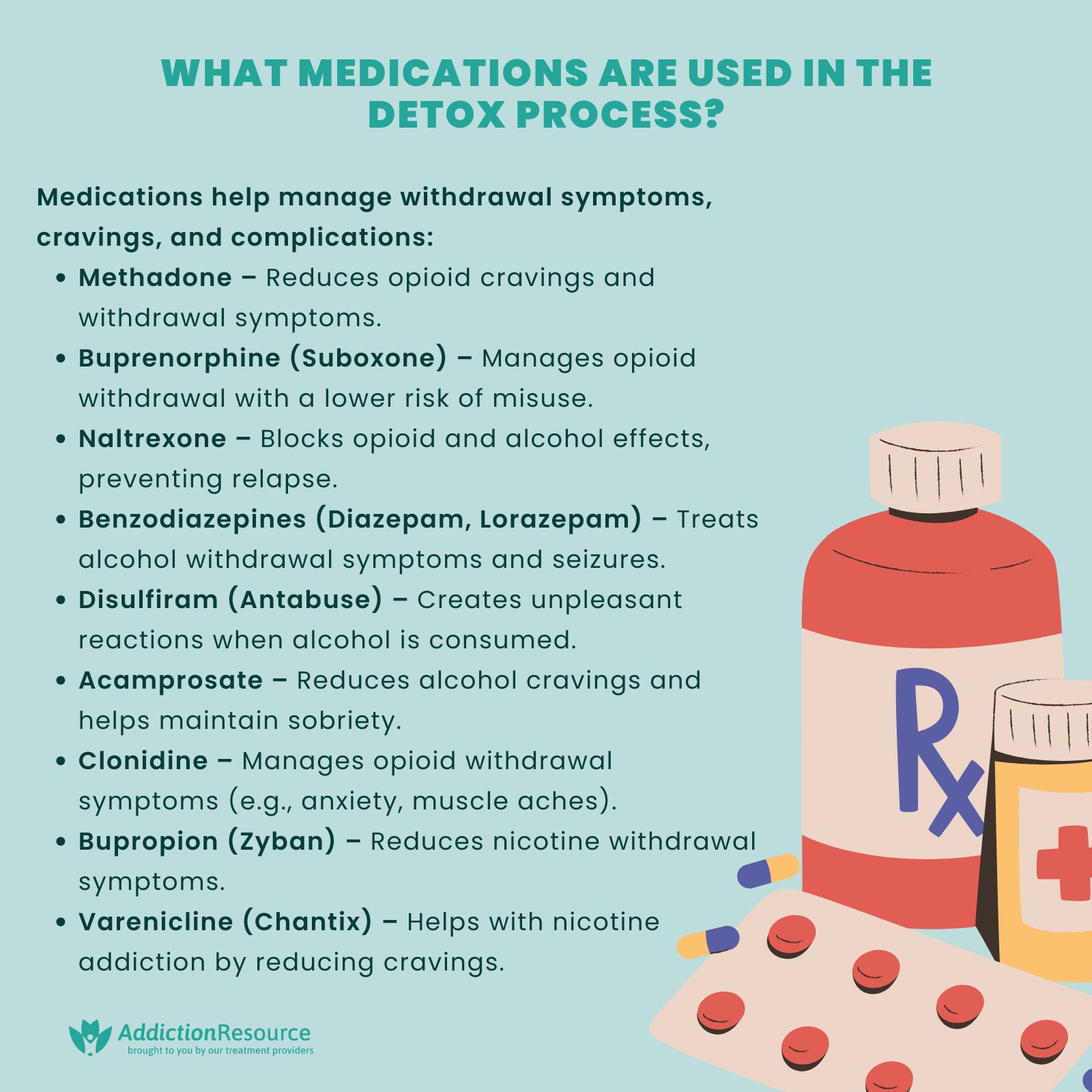
The medications are commonly used during detox to reduce withdrawal symptoms, prevent complications, and ease cravings. For opioid withdrawal, buprenorphine and methadone help minimize discomfort and stabilize brain chemistry. Benzodiazepines, such as diazepam or lorazepam, are prescribed for alcohol and sedative withdrawal to prevent seizures and manage anxiety. Other medications like clonidine or gabapentin are used to treat symptoms such as agitation, insomnia, or muscle pain. Medication-assisted detox improves safety and increases the likelihood of a successful transition into further treatment.
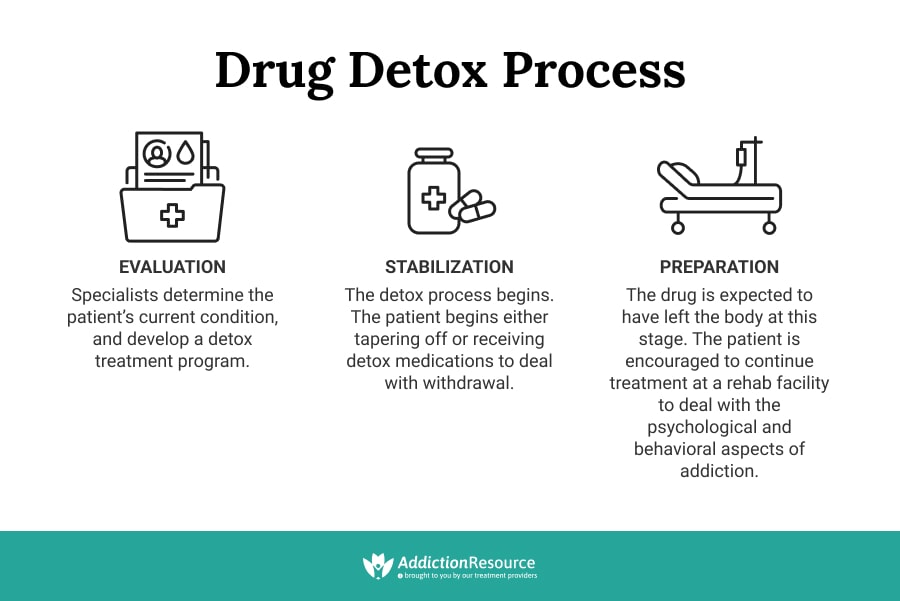
The detox process involves three key stages: evaluation, stabilization, and preparation for further treatment. During evaluation, medical professionals assess the individual’s physical and mental health, substance use history, and withdrawal risks. Stabilization involves medical monitoring, symptom management, and psychological support to ensure the patient remains safe and as comfortable as possible. Once withdrawal symptoms subside, individuals are prepared for the next phase of recovery, such as inpatient rehab or outpatient therapy.
While detox is a necessary step, it comes with uncomfortable and sometimes severe side effects. Common withdrawal symptoms include nausea, sweating, muscle pain, irritability, and insomnia. More severe cases, especially in alcohol or benzodiazepine withdrawal, leads to hallucinations, seizures, or delirium tremens (DTs). The intensity and duration of withdrawal symptoms depend on the substance used, the length of addiction, and individual health factors. Medical supervision is crucial to manage these effects and prevent serious complications.
Table of Contents:

What is Drug Detox?
Drug detox is a medically supervised process designed to safely manage acute withdrawal symptoms that occur when a person stops using addictive substances. Addiction is recognized as a brain disorder that alters neural pathways, making it difficult to quit without medical intervention. According to PubMed Central approximately 18% of treatment admissions for individuals aged 12 and older involved detoxification services.
Also known as medically supervised withdrawal, detox is the first step in recovery, ensuring that individuals clear substances from their system under professional care. While detox alone is not a complete treatment for addiction, it provides a foundation for long-term recovery by stabilizing individuals and preparing them for further care, such as medication-assisted treatment, therapy, or residential rehabilitation.
How long does drug detox take?
The detox process typically lasts between 3 to 10 days, depending on the substance used, the severity of dependence, and individual health factors. Some cases require a longer detox period, especially for benzodiazepines, alcohol, or opioids. It is important to understand how long detox lasts in order to plan for treatment.
Is drug detox safe?
Yes, when conducted in a medical setting, detox is safe and closely monitored. However, attempting to detox at home can be dangerous, especially for substances like alcohol, opioids, and benzodiazepines, which causes life-threatening withdrawal symptoms.
What are the 4 Types of Drug Detox?
The four types of drug detox include medical detox, rapid detox, outpatient detox, and social detox. Addiction disorders vary based on the drug used, how long it is used, and a person’s past medical history. These variables determine the course of the substance detox. Over the years, medical professionals have worked diligently to offer innovative detox options.
The available medical detox options include:
Medical Detox
Using medications to control the symptoms of withdrawal depends on the substance and severity of the symptoms. For example, in patients with alcohol dependence already suffering the most extreme forms of withdrawal, which are seizures and/or delirium, the administration of the medication should be carried out as soon as possible.
In some cases, individuals with substance dependency are hospitalized for other health issues and require hospital-based detoxification even if they weren’t seeking substance addiction therapy. Medical drug detox is done in inpatient facilities and is mainly limited to those with severe drug addictions.
Rapid and Ultra-Rapid Detoxification
The rapid or ultrarapid methods were designed to make the detoxification process shorter and easier.
During rapid substance detoxification, the patient is put under anesthesia and given medication to initiate the withdrawal process. The aim is to maintain the patient sedated until the withdrawal symptoms subside. However, warnings have been issued regarding the safety of this method.
Common narcotics antagonists such as naloxone, naltrexone, or nalmefene are used to induce narcotic withdrawal by displacing external opioids from receptor sites, promoting the detoxification process. Between 1996 and June 2014, 152,283 people received naloxone kits, leading to 26,463 reported overdose reversals according to “Take Home Naloxone Program” published by Wikimania. Although this type of drug detox was widely used in the 90’s, there are no controlled trials to assess the risk/benefit ratio. The rapid and ultra-rapid detoxes are still disputable.
Outpatient Detox Programs
Those with less severe dependence and stable homes undergo detoxification while living in their own homes. Medical professionals perform regular check-ins to monitor progress, adjust treatment plans, and provide guidance.
Social Detox
Social detox programs serve as short-term, nonmedical treatment services for people with less severe substance dependencies that do not require intensive medical supervision. These detox programs greatly vary in approach and scope.
Social drug detox programs differ in supervision levels, from on-site medical support to access through clinics, ‘cold turkey’ detox, or supervised medication. Regardless, these programs prioritize addressing psychological aspects, offering counseling, therapy, and peer support.
What Medications Are Used in the Detox Process?
The medications used in the detox process are carefully selected to manage withdrawal symptoms and reduce cravings, facilitating a safer and more comfortable transition to sobriety. These medications vary depending on the substance of abuse and individual patient needs.
The medications used in the detox process include:
Methadone
A long-acting opioid agonist used to reduce cravings and withdrawal symptoms in individuals detoxifying from opioids such as heroin or prescription painkillers. According to the National Institute on Drug Abuse (NIDA), patients stabilized on methadone, sustained doses of methadone can maintain employment, reduce criminal activity, and lower the risk of HIV and Hepatitis C transmission.
Buprenorphine
A partial opioid agonist that helps alleviate withdrawal symptoms and cravings. It has a ceiling effect, reducing the risk of misuse and respiratory depression. According to NIDA, buprenorphine treatment has retention rates averaging 57% at 90 days, demonstrating its effectiveness in sustaining treatment engagement.
Naltrexone
An opioid antagonist that blocks the euphoric effects of opioids and alcohol. It is used after detoxification to prevent relapse. According to NIDA, naltrexone reduces the risk of relapse in alcohol dependence by approximately 36% in the first three months.
Benzodiazepines
Medications such as diazepam or lorazepam are commonly used to manage alcohol withdrawal symptoms, including anxiety, seizures, and delirium tremens (DTs). These benzodiazepines are considered the gold standard for alcohol detoxification according to the National Library of Medicine.
Disulfiram (Antabuse)
Used in alcohol addiction treatment, disulfiram causes unpleasant reactions when alcohol is consumed, acting as a deterrent. Compliance can be challenging due to the severity of these reactions. According to SAMHSA, disulfiram is most effective when combined with behavioral therapy and support programs.
Acamprosate
A medication that reduces cravings and helps maintain abstinence in individuals recovering from alcohol dependence. It is particularly effective for those with severe alcohol use disorder. According to NIAAA, acamprosate increases the likelihood of sustained sobriety by 10-20% when combined with therapy.
Clonidine
An alpha-2 adrenergic agonist used to manage symptoms such as anxiety, agitation, muscle aches, and sweating during opioid withdrawal. It does not reduce cravings but is effective in easing physical discomfort during detox.
Bupropion (Zyban)
An atypical antidepressant that has been FDA-approved for smoking cessation. It reduces cravings and withdrawal symptoms associated with nicotine addiction. According to the CDC, bupropion increases quit rates by approximately 49% compared to placebo treatments.
Varenicline (Chantix)
A partial agonist at nicotinic acetylcholine receptors, used to reduce cravings and withdrawal symptoms in nicotine addiction. According to the American Lung Association, varenicline is nearly twice as effective as nicotine replacement therapy for long-term smoking cessation.
What are Withdrawal Symptoms?
The withdrawal symptoms vary for different drugs. Similar to the way substances cause different stimuli in people, so do withdrawal symptoms. Each substance has a withdrawal profile that varies in severity and between individuals. Withdrawal symptoms present in the most common addictive substances include:
| Substance | Withdrawal Symptoms |
| Alcohol | Anxiety, tremors, nausea, sweating, irritability, insomnia, hallucinations, seizures (in severe cases). |
| Marijuana/THC | Irritability, insomnia, loss of appetite, mood swings, restlessness. |
| Opioids | Nausea, vomiting, muscle aches, anxiety, insomnia, yawning, diarrhea, sweating, dilated pupils. |
| Sedatives | Anxiety, tremors, insomnia, seizures (in severe cases), irritability. |
| Stimulants | Fatigue, depression, increased appetite, disrupted sleep patterns, irritability. |
| Inhalants/Solvents | Nausea, headaches, dizziness, irritability, muscle weakness, tremors. |
| Nicotine | Irritability, anxiety, restlessness, increased appetite, insomnia. |
| Hallucinogens | No significant physical withdrawal; psychological symptoms include mood swings, flashbacks or anxiety. |
What is the 3-Step Drug Detox Process?
The 3 step drug detox process includes evaluations, stabilization and preparation. Providing a safe discontinuation from a substance of dependence is one of the main objectives of detox. Detoxification typically takes a few days (7 days) to a few weeks, depending on the substance, the level of dependence, and the patient’s access to assistance.
Health professionals should carefully follow the following steps:
Evaluation
An evaluation is the starting point before substance detox since it allows addiction specialists to assess the patient’s physical and mental health to provide more individualized treatment.
The evaluation examines the patient’s health, including any pre-existing or existing conditions (i.e., pregnancy, heart disease, diabetes, and mental health). Drug tests estimate the quantity of substances present in the patient’s system. This evaluation step assists professionals in determining whether medication-assisted detoxification is needed.
Stabilization
At this point, the patient progressively decreases the drug dose and experiences withdrawal symptoms as the body tries to reach a state of stability in the absence of the chemical. This step is unique to each patient and changes according to the intensity of their substance use.
Gradually reducing the drug dose assists in managing withdrawal symptoms while also protecting the patient’s mental and physical health.
Preparation
This is the final step of drug detox, where the chemicals are expected to have left the body.
Patients receive education about how detoxification is only the first part of the treatment process and that continued treatment is necessary. This stage helps patients develop coping mechanisms, skills and strategies to avoid relapse. According to Timko, C et. al. 2016 titled “Transitioning from Detoxification to Substance Use Disorder Treatment: Facilitators and Barriers” 49.9% of patients who underwent detoxification transitioned into substance use disorder treatment programs.
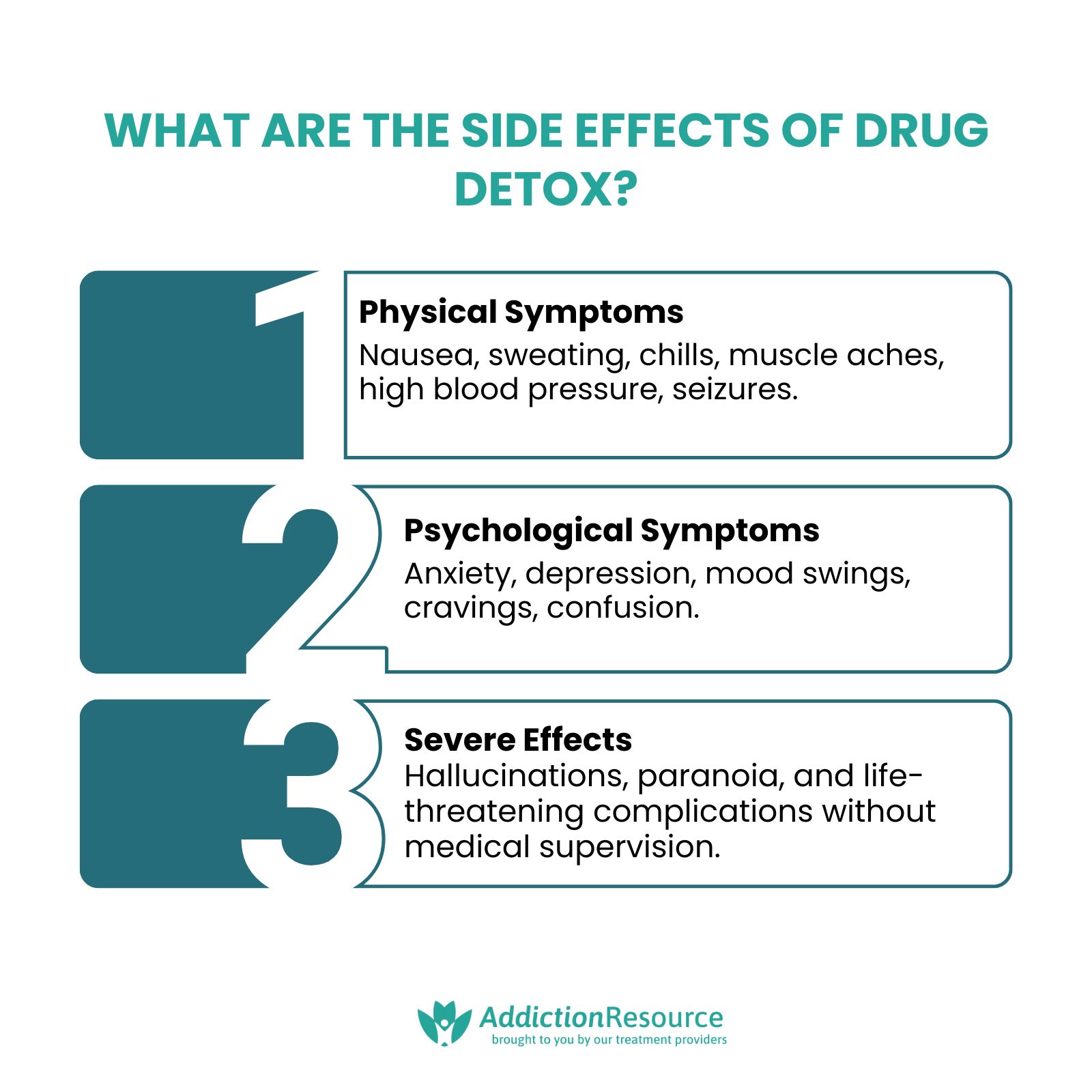
What are the Side Effects of Drug Detox?
The side effects of drug detox vary based on the substance used, the severity of addiction, and individual health factors. Withdrawal symptoms are mild to severe and include:
- Physical Symptoms: Nausea, vomiting, sweating, chills, muscle aches, headaches, tremors, rapid heart rate, high blood pressure, and seizures (in severe cases).
- Psychological Symptoms: Anxiety, depression, irritability, mood swings, confusion, agitation, and intense drug cravings.
- Severe Withdrawal Effects: Hallucinations, paranoia, delirium tremens (DTs) for alcohol withdrawal, and life-threatening complications without medical supervision.
Medical detox helps manage these symptoms safely, using medications and professional monitoring to reduce discomfort and prevent serious health risks.
What Comes After Substance Detox?
After drug detox, individuals transition into structured treatment and support programs to maintain sobriety and prevent relapse. Detox is only the first step, and ongoing care is essential for long-term recovery.
Inpatient Rehab
A structured, live-in treatment program that provides 24/7 medical and therapeutic support in a controlled environment. Inpatient rehab helps individuals develop coping skills, address underlying trauma, and build a strong foundation for sobriety through individual therapy, group counseling, and holistic wellness activities.
Partial Hospitalization Program (PHP)
A highly structured treatment option where individuals receive intensive therapy, medical monitoring, and support during the day but return home or to a sober living environment at night. PHP is ideal for those who need a high level of care but do not require 24/7 supervision.
Intensive Outpatient Program (IOP)
A flexible treatment model that allows individuals to attend therapy and support groups multiple times per week while maintaining work, school, or family commitments. IOP helps reinforce coping skills, provides continued support, and helps individuals transition into independent recovery.
Behavioral Therapies
Evidence-based approaches such as Cognitive Behavioral Therapy (CBT), Dialectical Behavior Therapy (DBT), and Motivational Interviewing (MI) help individuals identify triggers, change destructive thought patterns, and develop healthier coping mechanisms. Behavioral therapy plays a crucial role in preventing relapse and managing long-term recovery.
Medication-Assisted Treatment (MAT)
The use of FDA-approved medications such as methadone, buprenorphine, and naltrexone to reduce cravings, prevent withdrawal symptoms, and lower the risk of relapse. MAT is combined with therapy to address both the physical and psychological aspects of addiction.
Sober Living Homes
A drug- and alcohol-free residence designed to support individuals transitioning from treatment to independent living. Sober living homes provide structure, peer accountability, and ongoing recovery support while allowing individuals to gradually reintegrate into daily life.
12-Step and Peer Support Groups
Programs such as Alcoholics Anonymous (AA), Narcotics Anonymous (NA), and SMART Recovery provide peer support, mentorship, and a structured recovery framework. Regular attendance at 12 step meetings helps individuals stay connected to a sober community and maintain motivation for long-term recovery.
Family Therapy and Support
Addiction affects not only the individual but also their loved ones. Family therapy helps rebuild trust, improve communication, and educate family members on how to support recovery. Programs include family counseling sessions, educational workshops, and structured support groups.
Outpatient Therapy and Counseling
Continued one-on-one and group therapy sessions to address the emotional and psychological challenges of recovery. Outpatient therapy provides ongoing guidance, relapse prevention strategies, and mental health support to help individuals maintain long-term sobriety.
Relapse Prevention Planning
A personalized strategy that helps individuals identify triggers, develop coping techniques, and create a support system to prevent relapse. Relapse prevention plans include continued therapy, peer support meetings, lifestyle changes, and stress management techniques.
What does it mean to Taper off of Drugs?
Tapering off drugs refers to the gradual reduction of a substance under medical supervision to minimize withdrawal symptoms and reduce the risk of relapse. Instead of quitting abruptly (cold turkey), tapering involves slowly decreasing the dosage over a period of weeks or months, allowing the body to adjust to lower levels of the drug.
Tapering is commonly used for opioids, benzodiazepines, antidepressants, and certain stimulants, as stopping these substances suddenly leads to severe withdrawal symptoms, increased cravings, and potential medical complications.
A tapering schedule is typically customized based on the individual’s substance use history, dosage, and overall health. Medical professionals monitor the process closely, prescribing long-acting medications or supportive treatments to ease withdrawal discomfort and prevent relapse.
How do you prevent withdrawal symptoms?
Preventing withdrawal symptoms involves medical drug detox, gradually tapering off the substance while managing symptoms. Medications are prescribed to ease discomfort, guaranteeing a safe discontinuation and an effective withdrawal course.
Can I detox at home?
Yes you can detox at home however detoxing at home is not recommended, especially for substances with severe withdrawal risks. Medical supervision ensures safety by monitoring symptoms, providing medication when needed, and preventing dangerous complications.
What if I relapse after detox?
If you relapse after detox, individuals should re-enter treatment. Relapse is always a possibility, but continued treatment, therapy, and relapse prevention planning help reduce the risk. The National Institute on Drug Abuse (NIDA) suggests that 40% to 60% of individuals treated for substance use disorders relapse within a year. These statistics highlight the challenges in maintaining long-term sobriety and underscore the importance of comprehensive, ongoing treatment strategies.
Is there a rehab locator to help me find detox centers near me?
Yes, to find substance detox centers or rehabilitation facilities near you, there are many resources that help you find what you need. There are rehab locators and some other ways to find a detox center near you including:
- Use the SAMHSA Treatment Locator: Visit the Substance Abuse and Mental Health Services Administration (SAMHSA) website to search for licensed detox centers by zip code.
- Search Online Directories: Websites like Addiction Resource include directories of many different centers that are tailored to your needs.
- Contact Your Insurance Provider: Call your health insurance company to get a list of covered detox facilities in your area.
- Ask a Medical Professional: Your primary care doctor, therapist, or local hospital can provide referrals to reputable detox programs.
- Call a Helpline: National hotlines like SAMHSA’s Helpline (1-800-662-HELP) or local addiction recovery organizations can help connect you with nearby facilities.
- Check Local Community Resources: Many community health centers, non-profits, and support groups offer referrals to state-funded or private detox programs.
Find Drug Rehabilitation Centers Near You Anywhere In the US
Addiction Resource team has compiled an extensive list of the top drug rehabilitation facilities around the country. Use our locator tool to find the best centers near you.
Page Sources
- SAMHSA Releases New Data on Recovery from Substance Use and Mental Health Problems Among Adults in the United States. (2023, September 20). SAMHSA.
- Drug Misuse and Addiction | National Institute on Drug Abuse. (2024, January 5). National Institute on Drug Abuse.
- Zhu, H., & Wu, T. (2018). National trends and characteristics of inpatient detoxification for drug use disorders in the United States. BMC Public Health, 18.
- Substance Abuse and Mental Health Services Administration (US). (2006). 4 Physical detoxification services for withdrawal from specific substances. Detoxification and Substance Abuse Treatment - NCBI Bookshelf.
- Gowing, L., Ali, R., & White, J. M. (2006). Opioid antagonists under heavy sedation or anaesthesia for opioid withdrawal. Cochrane Database of Systematic Reviews.
- Gupta, M., Gokarakonda, S. B., & Attia, F. N. (2023, April 29). Withdrawal syndromes. StatPearls - NCBI Bookshelf.https://www.ncbi.nlm.nih.gov/books/NBK459239/
- Diaper, A. M., Law, F. D., & Melichar, J. K. (2014). Pharmacological strategies for detoxification. British Journal of Clinical Pharmacology, 77(2), 302-314. /li>


 Reviewed by:
Reviewed by:  Written by:
Written by: 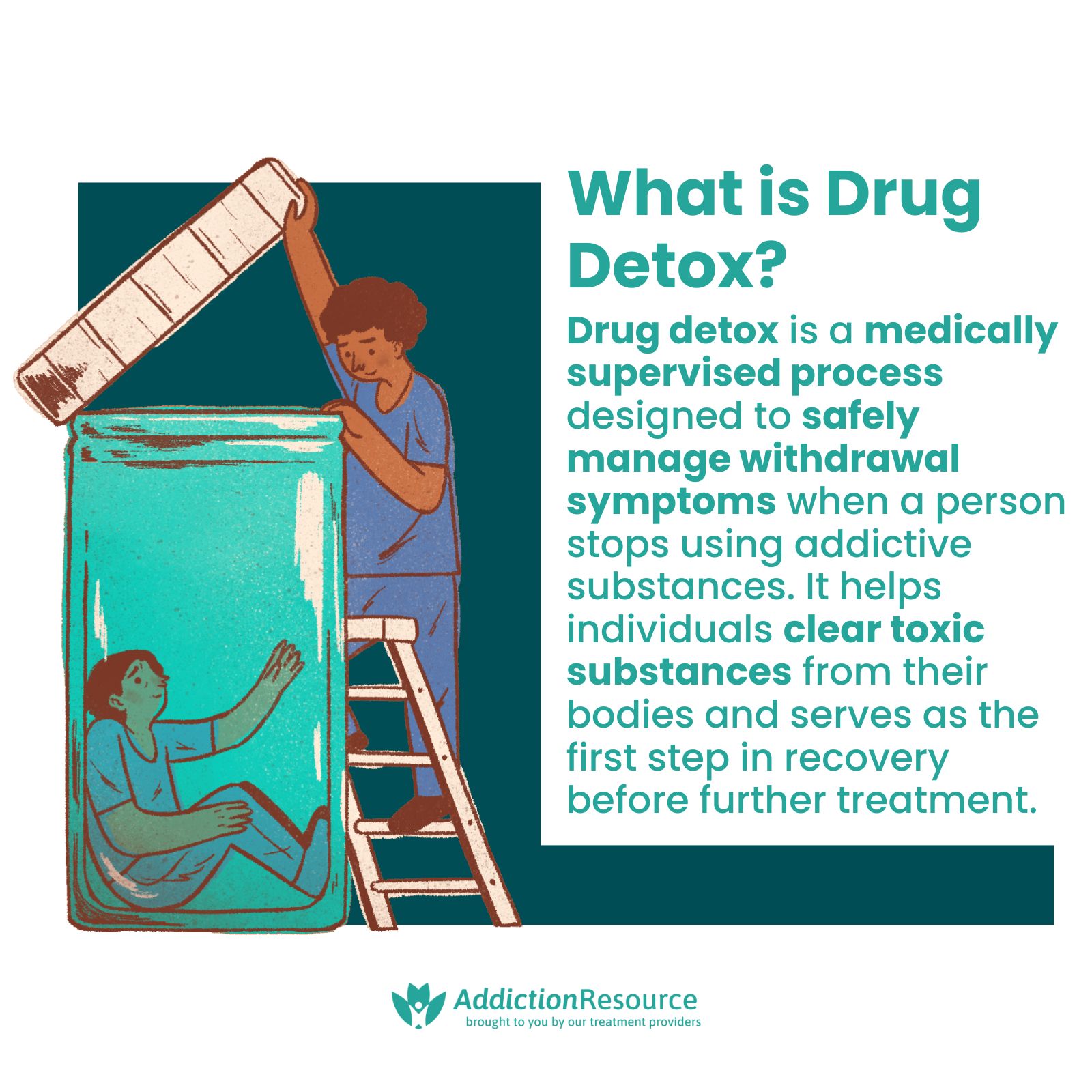


 FindTreatment.gov
FindTreatment.gov