Xanax addiction occurs when individuals develop a dependency on the medication due to misuse or prolonged use. This prescription drug is used to treat anxiety and panic disorders but becomes addictive when used outside prescribed guidelines. Xanax abuse involves taking higher doses or using the drug without a prescription, leading to physical and psychological dependence.
The main symptoms of Xanax addiction include drowsiness, slurred speech, impaired coordination, and memory problems. Individuals also experience mood swings, anxiety, and cravings for the drug. Over time, these symptoms worsen, affecting daily functioning and relationships.
Several factors contribute to the development of Xanax abuse, including a history of mental health disorders and high levels of stress. People with anxiety disorders or co-occurring conditions are at a higher risk, making them more vulnerable to becoming dependent on Xanax.
Table Of Contents:
The side effects of Xanax addiction are severe and life-threatening. These include respiratory depression, increased risk of overdose, depression, and withdrawal symptoms. The longer Xanax is misused, the higher the chance of experiencing these dangerous effects.
Treatment for Xanax addiction includes medical detoxification, cognitive behavioral therapy (CBT), and support groups. Gradual tapering of the drug under medical supervision is necessary to manage withdrawal symptoms. Medication-assisted treatment (MAT) is also used to help individuals recover and avoid relapse, with inpatient treatment programs offering additional support in some cases.
What is Xanax Addiction?
Xanax addiction is the compulsive use of alprazolam (Xanax), a medication in the benzodiazepine class prescribed for anxiety and panic disorders, as defined by Addiction Help. Xanax addiction occurs when individuals misuse the drug to achieve a sense of euphoria, leading to physical and psychological dependence. The drug’s calming and sedative effects are highly addictive, particularly when taken in larger-than-prescribed doses or without a prescription.
According to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), Xanax addiction falls under the category of “Substance Use Disorder” (SUD), which is characterized by a pattern of substance use leading to significant impairment or distress. The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5®) categorizes Xanax addiction as a sedative, hypnotic, or anxiolytic use disorder. It is considered an anxiolytic. Sedatives, hypnotics, and anxiolytics are substances that provide a calming or sleep-inducing effect. This includes symptoms such as using Xanax in larger amounts or over a longer period than intended, inability to control use, and cravings.
In the United States, benzodiazepine misuse, including Xanax, is a major public health concern. About 30.5 million adults use benzodiazepines, and of these, 5.3 million engage in misuse. Misuse rates of Xanax addiction are especially concerning, with an estimated 1.4% of the U.S. population reporting benzodiazepine misuse, which includes Xanax, as reported by AddictionHelp. Demographically, misuse of Xanax is more common among individuals aged 18-25 and those with a history of anxiety or other mood disorders.
The prevalence of Xanax addiction has surged, with emergency room visits related to recreational abuse rising from 57,419 in 2005 to 124,902 in 2010. Meanwhile, the number of prescriptions for Xanax increased from 38 million in 2006 to 50 million in 2013, reflecting a steady annual prescription growth rate of 9% since 2008, according to Drugs.com. Misuse for non-medical reasons, such as getting high or coping with stress, accounts for a large portion of the Xanax addiction cases.
Why Is Xanax Addictive?
Xanax is addictive because it affects the brain’s neurotransmitter systems, particularly by enhancing the activity of gamma-aminobutyric acid (GABA), a chemical that inhibits brain activity and produces calming effects. When taken, Xanax is rapidly absorbed into the bloodstream and reaches peak effects within an hour, creating feelings of euphoria, relaxation, and reduced anxiety. This rapid onset and intense effect make it highly reinforcing, leading individuals to misuse it to replicate these feelings.
Over time, the brain becomes tolerant to Xanax, requiring higher doses to achieve the same effects, which results in physical and psychological dependence. Studies have shown that prolonged use of benzodiazepines like Xanax alters brain chemistry, further increasing the risk of addiction, according to a study by Kang, M., Galuska, M. A., & Ghassemzadeh, S. et al. 2018, titled “Benzodiazepine toxicity.” The addictive potential of Xanax is further compounded when it is misused, as many individuals take it without medical supervision, combining it with other substances like alcohol or opioids for enhanced effects.
How is Xanax Consumed?
Xanax is consumed orally, in the form of tablets, and is ingested with or without food. The standard prescribed dosage for adults with anxiety or panic disorders starts at 0.25 mg to 0.5 mg, taken 2 to 3 times daily, according to Drugs.com. Adjustments are made to Xanax dosage based on individual needs and tolerance, up to a maximum daily dose of 4 mg. Xanax is absorbed quickly in the body, with peak effects felt within 1 to 2 hours of ingestion. However, some individuals misuse Xanax by crushing and snorting it or combining it with alcohol or other drugs to intensify its effects, which increases the risk of addiction and overdose.
What are the Signs Symptoms of Xanax Addiction?

The signs and symptoms of Xanax addiction are drowsiness, slurred speech, impaired coordination, and craving for Xanax. These symptoms affect both the physical and psychological aspects of an individual’s health. These signs are indicative of growing dependence on the drug and escalate in severity as addiction worsens.
These signs and symptoms of Xanax addiction are listed below:
- Drowsiness: Drowsiness is a common physical symptom of Xanax addiction, as it is a sedative that induces feelings of relaxation and sleepiness. Individuals experience excessive drowsiness even in situations where alertness is required, such as at work or while driving. This occurs because the brain becomes reliant on Xanax to manage anxiety and induces a state of lethargy, resulting in a disruption of daily functioning. According to GoodRx, about 3 out of 4 people taking alprazolam for panic disorder reported drowsiness.
- Slurred Speech: Slurred speech is a physical symptom that occurs when the central nervous system is overly suppressed due to Xanax abuse. This symptom is caused by the drug’s sedative effect on the brain, which impairs motor control and cognitive functions necessary for clear speech. As tolerance to the drug increases, slurred speech becomes more frequent, indicating a deeper dependence.
- Impaired Coordination: Impaired coordination is a physical symptom in which an individual experiences difficulty with balance, movement, or fine motor skills. It occurs because Xanax depresses the central nervous system, which in turn impairs the brain’s ability to control muscle movements effectively. The severity ranges from mild clumsiness to complete loss of motor control, especially as addiction worsens.
- Blurred Vision: Blurred vision is another physical symptom associated with Xanax addiction, occurring when the drug affects the visual processing centers of the brain. As a benzodiazepine, Xanax lowers blood pressure and slows down neural responses, leading to temporary vision disturbances. Long-term use increases the likelihood of experiencing chronic issues with vision. According to a study by Stafanous SN, Clarke MP, Ashton H, Mitchell KW. et al. 1999, titled “The effect of long-term use of benzodiazepines on the eye and retina,” 63.3% of patients complain of symptoms of irritation, blurred vision, or difficulty in reading while using Benzodiazepine, including Xanax.
- Cravings for Xanax: Cravings for Xanax are a psychological symptom of addiction. These occur as the brain becomes conditioned to expect the euphoric and calming effects of the drug. Individuals experience intense urges to take Xanax, leading to misuse or taking larger doses than prescribed. This symptom reflects the cycle of addiction and the body’s need to maintain the effects of the drug.
- Loss of Control: Loss of control is a psychological symptom where an individual feels unable to stop taking Xanax despite understanding its harmful effects. This symptom is a hallmark of addiction, as the person’s behavior becomes driven by the compulsive need to use the drug, even in situations where it causes harm. This is linked to changes in brain function and the development of dependency.
- Difficulty Concentrating: Difficulty concentrating is a psychological symptom that arises from the cognitive impairments caused by Xanax addiction. As the drug slows down neural activity, it impairs memory and the ability to focus. This symptom is common in both short-term use and chronic addiction, making it harder for individuals to perform tasks that require sustained attention.
- Lying to Get More Prescriptions: Lying to obtain more prescriptions is a behavioral symptom of Xanax addiction. As tolerance builds, individuals resort to dishonest practices, such as exaggerating symptoms to doctors or seeking prescriptions from multiple providers, in order to continue their drug use. This is a psychological manifestation of the obsession and compulsive behavior that comes with addiction.
Anxiety When Not Using the Drug: Anxiety when not using the drug is both a physical and psychological symptom. Xanax is used to manage anxiety, and over time, the body becomes reliant on it to maintain a sense of calm. When the drug is not available, the individual experiences heightened anxiety, which leads to withdrawal symptoms. This cycle of using the drug to avoid anxiety is a key feature of addiction. The most common symptom is a short-lived “rebound” anxiety and insomnia, coming on within 1-4 days of discontinuation, according to a study by Pétursson H. et al. 1994, titled “The benzodiazepine withdrawal syndrome.” The second pattern is the full-blown withdrawal syndrome, usually lasting 10-14 days; finally, a third pattern represents the return of anxiety symptoms, which then persist until some form of treatment is instituted.
What are the causes of Xanax Addiction?
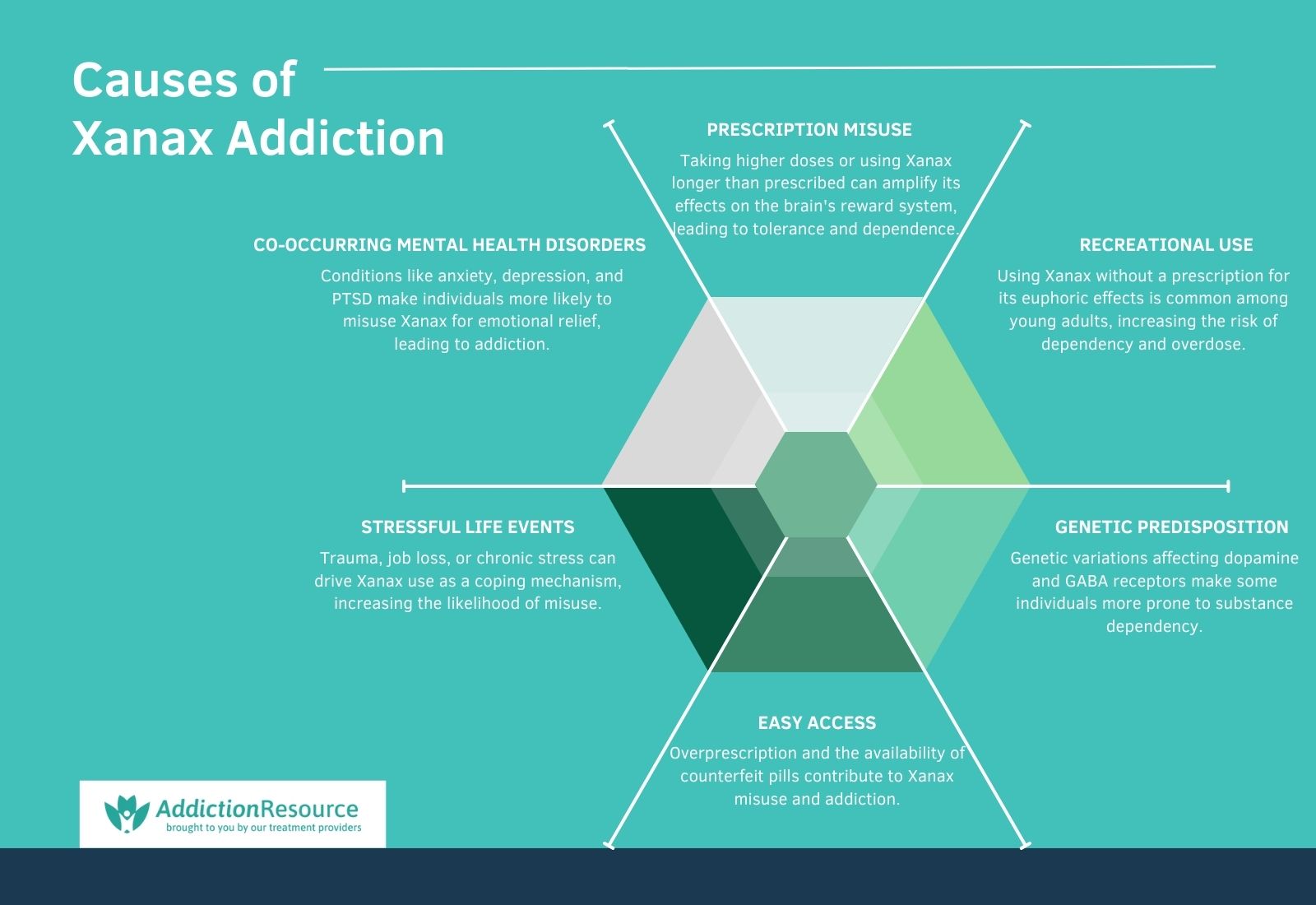
The causes of Xanax addiction are prescription misuse, recreational use, co-occurring mental health disorders, genetic predisposition, stressful life events, and easy access. These factors, individually or combined, contribute to the risk of dependence and addiction.
The causes of Xanax addiction are as follows:
- Prescription Misuse: Misusing a Xanax prescription, such as taking higher doses than prescribed or using it for longer durations, significantly increases the risk of addiction. This happens because overuse amplifies the drug’s effects on the brain’s reward system, leading to tolerance and dependence. Maust DT, Lin LA, and Blow FC conducted the study et al. 2019, titled “Benzodiazepine Use and Misuse Among Adults in the United States” found that 17.2% of benzodiazepine users, including Xanax, misused their prescriptions, with misuse being most common among younger adults (18–25).
- Recreational Use: Recreational use of Xanax involves taking the drug without a prescription or for non-medical reasons, such as achieving a euphoric high. This behavior is driven by the drug’s rapid action and potent calming effects, which reinforce misuse. Studies show that younger adults, particularly those aged 18-25, are at higher risk of recreational use, obtaining the drug from peers or illicit sources. According to recent data by Statista, over 17 million prescriptions for Xanax were dispensed in the U.S. in 2022, with young adults and women representing a large portion of problematic users of Xanax, including recreational use, which has contributed to rising rates of dependency and overdose.
- Co-occurring Mental Health Disorders: Individuals with conditions like anxiety, depression, or PTSD are more likely to develop Xanax addiction. These disorders lead to overreliance on the drug for emotional relief, making it difficult to discontinue use. A study published in Psychiatric Services found that individuals with anxiety disorders are twice as likely to misuse benzodiazepines compared to the general population.
Genetic Predisposition: Genetic factors play a role in determining an individual’s susceptibility to addiction. Variations in genes related to dopamine regulation and GABA receptors make certain individuals more prone to developing dependency on substances like Xanax. Research in addiction biology by Bevilacqua L, Goldman D. et al. 2009, titled “Genes and addictions,” has highlighted the heritability of substance use disorders, with genetic factors contributing to 40-60% of addiction risk. - Stressful Life Events: Stressful experiences, such as trauma, job loss, or relationship issues, trigger Xanax use as a coping mechanism. Chronic stress alters brain chemistry, making it more receptive to the soothing effects of benzodiazepines, which lead to misuse. Studies from the National Institute on Drug Abuse emphasize the link between stress and increased substance use, including benzodiazepines. The survey by Airagnes G, Lemogne C, et al. 2019, titled “Work-Related Stressors and Increased Risk of Benzodiazepine Long-Term Use: Findings From the CONSTANCE Population-Based Cohort,” found a significant association between work-related stress and long-term benzodiazepine use, including Xanax. Individuals who reported frequent exposure to stressful situations in public-facing jobs had higher odds of long-term use, with men showing a 2.2-fold increase and women a 1.6-fold increase compared to those with minimal exposure. The risk was dose-dependent, increasing with the frequency of stressful encounters. These findings persisted even after adjusting for factors like age, education, and health vulnerabilities, indicating that chronic stress directly contributes to the sustained use of benzodiazepines.
- Easy Access: The widespread availability of Xanax, both through legal prescriptions and illicit markets, contributes to its misuse. Overprescription by healthcare providers and the availability of counterfeit pills online has made it easier for individuals to obtain and misuse the drug. The U.S. has seen a steady rise in prescriptions for benzodiazepines, with Xanax being one of the most frequently prescribed, fueling its accessibility and misuse. According to a report by Statista, Xanax prescriptions in the United States rose by approximately 61%, from 17.91 million in 2004 to a peak of 28.9 million in 2013. However, prescriptions have since declined, dropping by about 14% from 17.91 million in 2004 to 15.38 million in 2021. This trend reflects increased awareness and regulatory efforts to curb benzodiazepine overprescription. In 2022, it was the 41st most commonly prescribed medication in the United States.
Who is at Risk of Developing Xanax Addiction?
Individuals at risk of developing Xanax addiction include those with anxiety disorders, a family history of substance abuse, chronic stress, past trauma, or co-occurring mental health disorders such as depression. These factors significantly increase vulnerability to Xanax misuse and dependence, as individuals rely on the drug for emotional relief or to cope with persistent psychological challenges.
The following individuals are at risk of developing Xanax addiction:
- Individuals with anxiety disorders: People with anxiety disorders are prescribed Xanax for symptom management, making them highly susceptible to dependence. A study by Addiction Help indicates that those with anxiety are twice as likely to misuse benzodiazepines compared to the general population, as they rely on the drug to manage chronic symptoms.
- People with a family history of substance abuse: A genetic predisposition to addiction places individuals with a family history of substance abuse at greater risk. Research Koob GF, Volkow ND. et al. 2016, titled “Neurobiology of addiction: A neurocircuitry analysis,” shows that genetic factors account for 40-60% of the risk for addiction, making these individuals more likely to misuse Xanax if prescribed.
- Individuals with chronic stress: Chronic stress leads to Xanax misuse as individuals seek relief from persistent psychological pressure. A study by Airagnes G. et al. 2019 found that individuals in high-stress jobs were twice as likely to use benzodiazepines long-term, increasing the risk of addiction.
- People with co-occurring mental health disorders: Individuals with conditions like depression or PTSD are at increased risk of Xanax addiction. They have been prescribed Xanax for symptom relief, and the overlap of psychological conditions heightens their dependency risk. According to a study by Schmitz A. et al. 2016, titled “Benzodiazepine use, misuse, and abuse: A review,” approximately 40% of individuals with these mental health conditions report benzodiazepine misuse, highlighting their increased vulnerability.
- Individuals with a history of trauma: Trauma survivors frequently turn to substances like Xanax for coping, especially when dealing with PTSD. Studies suggest that trauma increases the likelihood of substance misuse by as much as 50%, underscoring the vulnerability of this group. A cross-sectional survey by Vogel M et al. 2011, titled “Prolonged use of benzodiazepines is associated with childhood trauma in opioid-maintained patients,” revealed a strong link between childhood trauma and prolonged benzodiazepine use, including Xanax. Among 193 patients with Benzo dependence, 67% reported at least one moderate-to-severe traumatic experience in childhood, such as emotional abuse, emotional neglect, or physical neglect.
- Those using Xanax without a prescription: Recreational users who obtain Xanax illicitly or through non-medical channels are at high risk of addiction. Misuse rates are particularly high among individuals aged 18-25, who seek the drug for its sedative effects.
- People with impulsive or risk-taking behaviors: Those with impulsive tendencies or a propensity for risky behaviors are more likely to misuse substances, including Xanax. Impulsivity is a well-documented risk factor for substance abuse disorders, increasing vulnerability to addiction.
- Individuals with long-term prescriptions for benzodiazepines: Long-term use of Xanax for medical reasons, such as managing chronic anxiety, leads to tolerance and physical dependence. According to the FDA, dependency risks increase significantly after 4-6 weeks of continuous use.
- Adolescents and young adults: Younger individuals, particularly those aged 18-25, are at higher risk of Xanax addiction due to experimentation and peer influence. Research by NIDA indicates that this age group accounts for the highest rates of misuse, at approximately 5% annually.
- People in high-pressure professions: Individuals in demanding fields, such as healthcare, law enforcement, or corporate roles, misuse Xanax to cope with stress and insomnia. High stress and easy access to prescriptions exacerbate the risk of addiction.
What are the side effects of Xanax Addiction?

The side effects of Xanax addiction are drowsiness, confusion, and memory problems, among others. These effects significantly impair physical and mental health, leading to long-term consequences.
These effects of Xanax addiction are explained below:
- Drowsiness: Drowsiness is a common side effect of Xanax addiction, caused by its sedative effect on the central nervous system (CNS). Xanax enhances the activity of gamma-aminobutyric acid (GABA), resulting in relaxation and reduced alertness. Chronic use leads to excessive daytime sleepiness, affecting productivity and safety. According to a study by Chen L et al. 2016, titled “ The association between benzodiazepine use and sleep quality in residential aged care facilities: a cross-sectional study,” 49.5% of chronic benzodiazepine users experience persistent drowsiness, even after stopping use compared to 55.3% of non-users.
- Confusion: Confusion arises due to Xanax’s impact on the brain’s cognitive processing. Prolonged use disrupts neurotransmitter balance, impairing decision-making and thought clarity. A study by Zetsen SPG et al. 2022, titled “Cognitive Functioning in Long-Term Benzodiazepine Users,” shows that up to 20.7% of long-term benzodiazepine users report cognitive dysfunction, including confusion. This effect is particularly dangerous for older adults, increasing the risk of accidents and poor quality of life.
Memory Problems: Memory impairment, particularly short-term memory loss, is another common side effect of Xanax addiction. Benzodiazepines suppress brain activity in the hippocampus, a region important for memory formation. Research by Chowdhury ZS et al. 2016, titled “The Effect of Chronic Alprazolam Intake on Memory, Attention, and Psychomotor Performance in Healthy Human Male Volunteers,” found that 50% of chronic users reported memory issues, with severity increasing with dosage and duration of use. - Slurred Speech: Slurred speech results from Xanax’s CNS depressant effects, which slow down motor coordination and muscle control. This is a sign of high doses or prolonged misuse. A study published in The Journal of Clinical Psychiatry highlights that 25% of users experience speech difficulties during dependency phases.
- Impaired Coordination: Impaired motor coordination occurs as Xanax affects the cerebellum, which is responsible for muscle control and movement. This leads to an increased risk of falls and accidents. According to the National Institute on Drug Abuse (NIDA), 20-40% of benzodiazepine users report coordination issues during prolonged use.
- Mood Swings: Mood swings are linked to the disruption of emotional regulation caused by Xanax addiction. Users experience intense highs and lows, exacerbating pre-existing mental health conditions.
- Depression: Depression develops with prolonged Xanax use, as the drug depletes serotonin levels over time. Benzodiazepine users, including Xanax, develop depressive symptoms, worsening with extended use.
- Anxiety: Paradoxically, Xanax addiction leads to rebound anxiety, where anxiety symptoms worsen during withdrawal or between doses. Xanax users report heightened anxiety during dependency phases, according to Healthline.
- Irritability: Irritability is a psychological side effect caused by withdrawal or fluctuating drug levels in the bloodstream. This symptom affects nearly half of the users in withdrawal phases, according to the Mayo Clinic.
- Nausea: Nausea is a common physical side effect due to Xanax’s impact on the gastrointestinal system. Persistent nausea affects around 30% of individuals during addiction phases, especially during withdrawal, according to Medical News Today.
- Dizziness: Dizziness occurs as a result of Xanax’s sedative effects on the brain, disrupting balance and spatial perception. WebMD indicates that 35% of users experience dizziness during addiction.
- Fatigue: Chronic fatigue is a side effect of prolonged CNS suppression by Xanax. This leads to reduced physical stamina and mental alertness, according to a study by Ait-Daoud N, Hamby AS, Sharma S, Blevins D. et al. 2018, “A Review of Alprazolam Use, Misuse, and Withdrawal.”
- Withdrawal Symptoms: Withdrawal symptoms, such as tremors, seizures, and anxiety, are severe effects of Xanax addiction. They occur when the body becomes dependent and struggles to function without the drug. One study by Zaman H., Gibson R.C., Walcott G., et al. 2019, titled “Benzodiazepines for catatonia in people with schizophrenia or other serious mental illnesses,” found a withdrawal rate of approximately 40% in those using for six or more months with abrupt cessation of Benzodiazepines including Xanax.
- Respiratory Issues: Respiratory depression is a dangerous side effect of Xanax addiction, especially when combined with other CNS depressants like alcohol. Prolonged use slows breathing, increasing the risk of hypoxia and overdose.
- Increased Risk of Overdose: Addiction increases the likelihood of overdose as tolerance builds, requiring higher doses to achieve the same effect. Benzodiazepines like Xanax contribute to a significant number of overdose deaths annually, especially when mixed with opioids or alcohol.
Hope Without Commitment
Find the best treatment options. Call our free and confidential helpline
Most private insurances accepted
How to Diagnose Xanax Addiction?
To diagnose Xanax addiction, healthcare providers conduct a comprehensive evaluation that includes a detailed medical history, psychological assessment, and an evaluation of the patient’s substance use patterns. They use diagnostic criteria outlined in the DSM-5 (Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition), which defines substance use disorder based on symptoms like compulsive use, inability to reduce or stop use, cravings, and continued use despite negative consequences. Tools like structured interviews, self-reported questionnaires, and toxicology screenings are also employed. Recognizing signs such as increased tolerance, withdrawal symptoms, and behavioral changes helps confirm the diagnosis. Early and accurate diagnosis is important for effective treatment planning.
What Tests Are Used to Diagnose Xanax Addiction?
The tests used to diagnose Xanax addiction include the DSM-5 criteria assessment, substance use questionnaires, urine drug screening, blood tests, and mental health evaluations, each offering unique insights into the nature and severity of the addiction.
The DSM-5 criteria assessment is a structured diagnostic approach used by healthcare providers to identify substance use disorders. It evaluates behaviors such as loss of control over use, cravings, tolerance, and withdrawal symptoms. This method is highly effective as it provides a standardized framework to diagnose addiction, ensuring consistency across clinical settings.
Substance use questionnaires, such as the AUDIT (Alcohol Use Disorders Identification Test) or ASSIST (Alcohol, Smoking, and Substance Involvement Screening Test), are self-reported tools that assess the frequency and impact of substance use. These questionnaires are non-invasive and easy to administer, offering valuable insights into a person’s relationship with Xanax and identifying patterns indicative of addiction.
Urine drug screening is a laboratory test that detects the presence of Xanax or its metabolites in the urine. It is commonly used because it is quick, cost-effective, and confirms recent use. However, it does not capture the frequency of use or dependency, making it more effective when combined with other diagnostic tools.
Blood tests also detect Xanax and its concentration in the bloodstream. While less commonly used due to higher costs and shorter detection windows compared to urine tests, blood tests are highly accurate and are important in determining the exact levels of the drug, especially in cases of suspected overdose or acute misuse.
Mental health evaluations are integral to understanding co-occurring conditions, such as anxiety, depression, or PTSD, that contribute to or result from Xanax addiction. These assessments involve interviews and validated screening tools, helping clinicians develop a holistic treatment plan tailored to the individual’s needs.
What are the Treatment Options for Xanax Addiction?
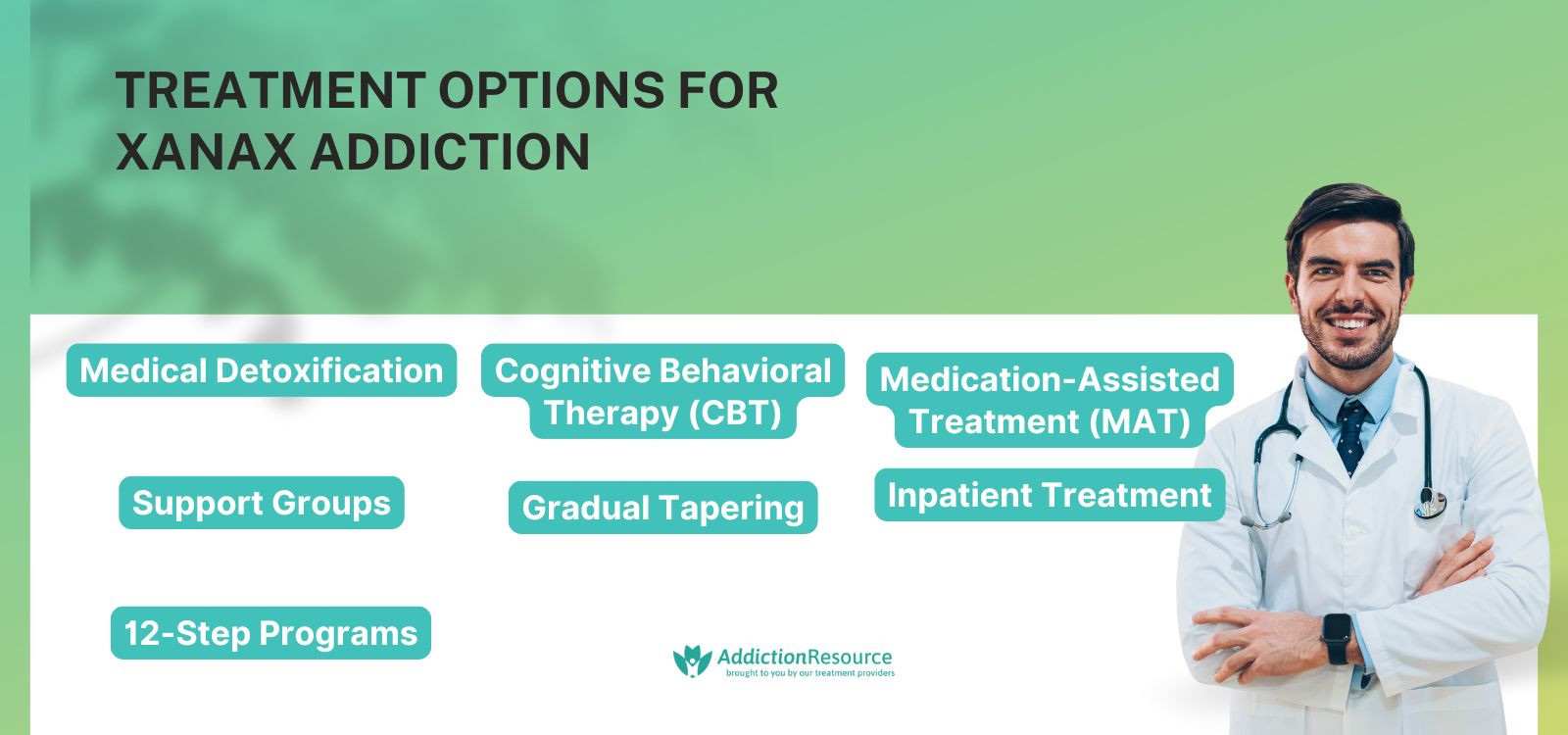
The treatment options for Xanax addiction include medical detoxification, cognitive behavioral therapy (CBT), medication-assisted treatment (MAT), support groups, gradual tapering, inpatient treatment, and 12-step programs. Each option addresses different aspects of addiction, offering a comprehensive approach to recovery.
The treatment options for Xanax addiction are as follows:
Medical Detoxification
Medical detox involves supervised withdrawal from Xanax, usually in a clinical setting. It reduces the risk of severe withdrawal symptoms like seizures by gradually weaning off the drug or using a substitute medication like diazepam. Medically supervised detox is safer and more effective than abrupt cessation, especially for long-term users. Recovery time varies but lasts 7–10 days for acute withdrawal, although post-acute symptoms persist longer, according to a study by Hood, S. D. et al. 2014, titled “Benzodiazepine dependence and its treatment with low dose flumazenil.” The advantages of medical detox are safety and medical oversight, but they are expensive and require a clinical facility.
Cognitive Behavioral Therapy (CBT)
CBT is a psychotherapeutic approach that helps individuals identify and change harmful thought patterns and behaviors related to Xanax use. It focuses on coping mechanisms and relapse prevention. CBT significantly improves long-term recovery outcomes when combined with other treatments. Recovery time depends on the individual’s progress but involves 12–16 sessions over several months. CBT is advantageous for addressing underlying psychological issues but requires consistent participation and commitment. Cognitive behavioral therapy (CBT) has been shown to be an effective treatment for addiction, with a study by Verywell Mind reporting success rates of around 60–67%.
Medication-Assisted Treatment (MAT)
MAT uses medications like flumazenil or antidepressants to manage withdrawal symptoms and cravings while stabilizing mental health conditions. Medication-assisted treatment (MAT) has demonstrated moderate success rates in addiction recovery, as reflected in a systematic review of 58 studies with 27,047 participants in low- and middle-income countries (LMICs) by Feelemyer J et al. 2014, titled “Retention of participants in medication-assisted programs in low- and middle-income countries: an international systematic review.” Medication-assisted treatment (MAT) for addiction recovery has shown success, with retention rates averaging 54% after 12 months of treatment. For those using buprenorphine, about 48% of participants stayed in treatment after a year, while 57% of methadone users continued their programs. Recovery time varies but complements other treatments over several months. While effective, it involves side effects and long-term medication dependence.
Support Groups
Support groups like Narcotics Anonymous or SMART Recovery provide peer support and shared experiences to help individuals stay committed to recovery. These groups offer emotional support, accountability, and community. Although they do not replace medical treatment, they are highly effective in maintaining sobriety. They are free and accessible but do not address medical or psychological issues directly.
Gradual Tapering
Gradual tapering involves slowly reducing the Xanax dosage under medical supervision to minimize withdrawal symptoms and dependency. Gradual tapering is a safer alternative to abrupt cessation, especially for long-term Xanax users. Tapering schedules vary but span weeks to months, depending on the individual’s dependency level. While highly effective, it requires patience and strict adherence to medical advice.
Inpatient Treatment
Inpatient treatment provides a structured environment for recovery, including medical care, therapy, and support. It is ideal for severe cases of addiction or individuals with co-occurring disorders. Inpatient programs improve outcomes due to the controlled environment and comprehensive care. Recovery time varies but usually lasts 30–90 days. According to the National Institute on Drug Abuse, 40–60% of people maintain sobriety after treatment. While effective, it is costly and requires a temporary commitment to living in a facility.
12-Step Programs
12-step programs like Alcoholics Anonymous (AA) adapt their model for substance abuse, emphasizing spiritual and personal growth through structured steps. These programs provide long-term support but work best when combined with medical and psychological treatments. The recovery timeline is indefinite, as these programs focus on lifelong sobriety. The advantage is their accessibility and community, though some individuals seek alternatives to the spiritual framework. People who went to 12-step meetings in the study had about a 75% success rate, according to Krentzman AR, Robinson EA et al. 2010, titled “How Alcoholics Anonymous (AA) and Narcotics Anonymous (NA) Work: Cross-Disciplinary Perspectives.”
What is Xanax?
Xanax, also known as alprazolam, is a prescription medication classified under the benzodiazepine class of drugs, primarily used to treat anxiety disorders, panic disorders, and sometimes generalized anxiety disorder (GAD). Approved by the U.S. Food and Drug Administration (FDA), Xanax acts as a central nervous system (CNS) depressant by enhancing the activity of gamma-aminobutyric acid (GABA), the brain’s primary inhibitory neurotransmitter, which produces calming effects. Defined by the National Cancer Institute, Xanax is “A drug used to treat anxiety disorders and panic attacks. It is being studied in the treatment of nausea and vomiting caused by some cancer treatments. It is a type of benzodiazepine. Also called alprazolam.” Its molecular structure includes a triazole ring fused to the benzodiazepine core, with a molecular formula of C17H13ClN4 and a molecular weight of approximately 308.76 g/mol.
Xanax works by binding to GABA-A receptors in the brain, enhancing their affinity for GABA, and increasing chloride ion influx into neurons. This hyperpolarizes the neuronal membrane, reducing neuronal excitability and producing calming and sedative effects. Its lipophilic nature allows rapid crossing of the blood-brain barrier, contributing to its quick onset of action and increased potential for tolerance and dependence with prolonged use, as noted by Drugwatch. While therapeutic doses effectively manage anxiety by mitigating excessive neural firing, higher doses or misuse result in drowsiness, memory impairment, or severe respiratory depression.
What is Xanax Withdrawal?
Xanax withdrawal is the physical and psychological symptoms that occur when an individual who has been using Xanax (alprazolam) regularly and in significant amounts reduces their dosage or stops taking the drug abruptly. As a benzodiazepine, Xanax affects gamma-aminobutyric acid (GABA) receptors in the brain, and prolonged use leads to dependence. When the drug is discontinued, the brain struggles to regulate neural activity, resulting in withdrawal symptoms. These symptoms range from mild anxiety and restlessness to severe complications like seizures, hallucinations, and delirium tremens in extreme cases.
What are Xanax Withdrawal Symptoms?
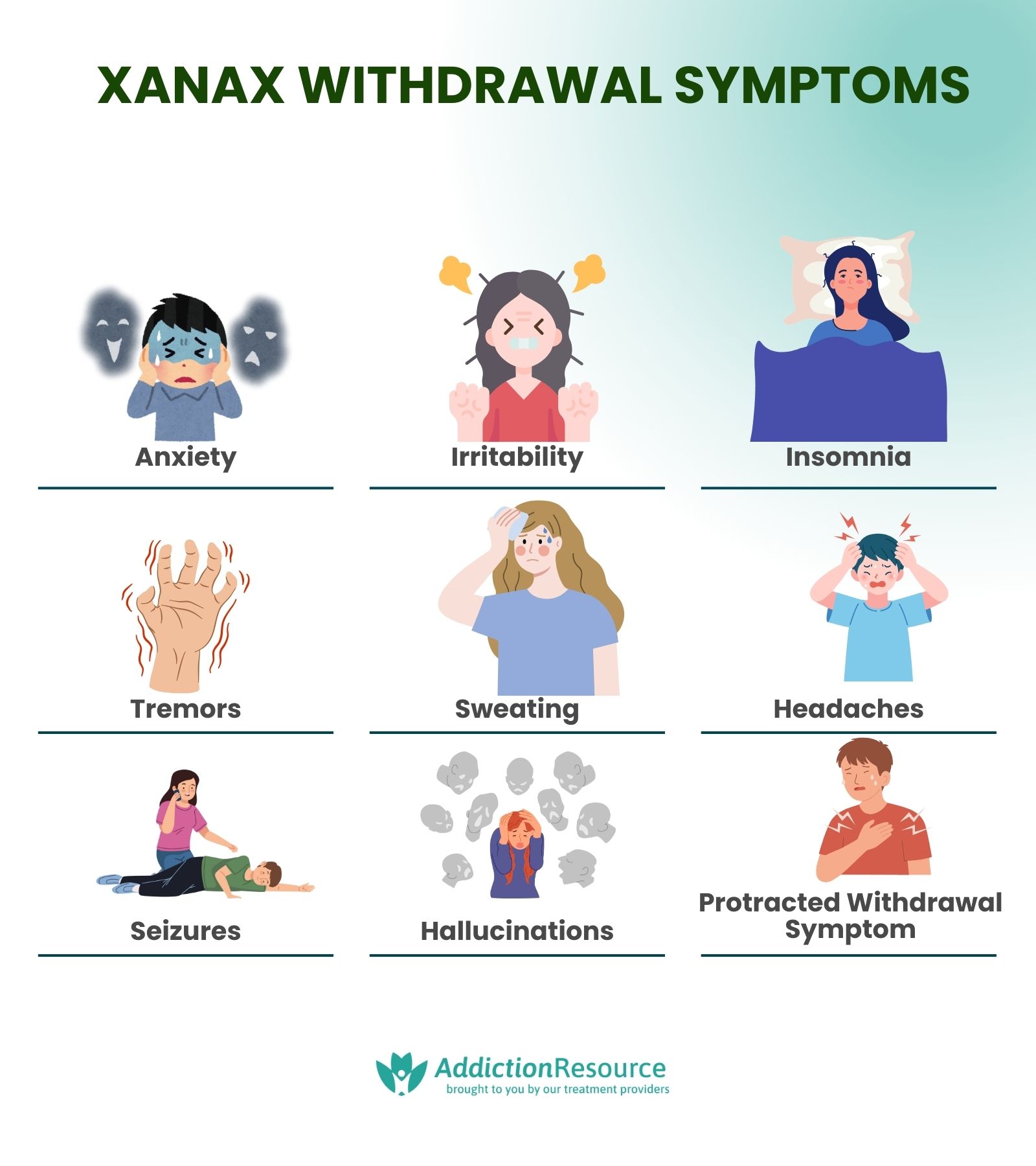
The Xanax withdrawal symptoms are anxiety, irritability, and insomnia. These symptoms occur when an individual stops using or reduces their dose of Xanax after prolonged use, reflecting the body’s physical and mental dependence on the drug. Withdrawal symptoms range from mild discomfort to severe complications, depending on the dosage and duration of use, as well as individual factors like overall health. According to Healthline, symptoms begin within hours to a day after cessation, peak by the second day, and persist for weeks. Abrupt cessation carries significant risks, including life-threatening seizures and respiratory distress, as highlighted in research by Brett J. and Murnion B. et al., 2015, titled “Management of benzodiazepine misuse and dependence.”
The Xanax withdrawal symptoms are as follows:
- Anxiety: A rebound increase in anxiety is one of the most common withdrawal symptoms. This occurs because Xanax suppresses excessive neural activity, and its absence leads to heightened nervous system activity. Anxiety during withdrawal is severe, mimicking or exceeding the initial condition for which Xanax was prescribed.
- Irritability: Irritability is another psychological symptom resulting from the brain’s struggle to regain chemical balance. During the withdrawal phase, this results in heightened emotional sensitivity and frustration.
- Insomnia: Xanax withdrawal disrupts sleep patterns, leading to difficulty falling or staying asleep. Insomnia persists for weeks and significantly impacts mood and physical recovery during withdrawal, according to Medical News Today in “Rebound Insomnia.”
- Tremors: Physical symptoms, such as hand or body tremors, are common. They result from the central nervous system’s overactivity after the calming effects of Xanax are removed. These tremors range from mild to severe.
- Sweating: Excessive sweating is a physical reaction linked to increased autonomic nervous system activity. This symptom accompanies anxiety and persists throughout withdrawal, as studied by Pétursson H. et al. 1994, in “The benzodiazepine withdrawal syndrome.”
- Headaches: Frequent headaches are another common symptom. They are caused by tension and neural overstimulation during the withdrawal process. Although usually temporary, they are debilitating.
- Seizures: In severe cases, withdrawal from Xanax leads to seizures, particularly in individuals who stop abruptly or use high doses. This symptom is life-threatening and requires immediate medical attention, according to a study by Noyes R Jr, Perry PJ, Crowe RR, Coryell WH, Clancy J, Yamada T, Gabel J., et al. 1986, titled “Seizures following the withdrawal of alprazolam.”
- Hallucinations and Delirium: Some individuals experience hallucinations or delirium during Xanax withdrawal, particularly in severe cases or without medical supervision. These symptoms indicate extreme neural dysregulation and necessitate urgent medical care. McKenzie RR Jr, Madadi P, Sharma TR, et al. 2014, in their research titled “Alprazolam withdrawal delirium and brief reversible psychosis: a case report,” studied the effects of Xanax withdrawal on a 33-year-old patient who experienced delirium and psychosis after discontinuing alprazolam use. The case revealed that withdrawal from alprazolam causes severe psychological symptoms, including hallucinations, agitation, and disorientation, even in the absence of typical withdrawal signs such as tremors or nausea.
- Protracted Withdrawal Symptoms: In some cases, withdrawal symptoms persist for weeks or months, known as protracted withdrawal. Symptoms include persistent anxiety, insomnia, and mood disturbances, significantly affecting quality of life. Studies indicate that between 10% and 25% of chronic benzodiazepine users experience protracted withdrawal when they stop taking the drug, according to a survey by Hood, S. D., Norman, A., Hince, D. A., Melichar, J. K., & Hulse, G. K. et al. 2014, titled “Benzodiazepine dependence and its treatment with low dose flumazenil.”
What is the Withdrawal Timeline of Xanax?
The withdrawal timeline of Xanax is characterized by a series of physical and psychological phases that vary in intensity. Withdrawal begins within hours of reducing or stopping Xanax use, with symptoms peaking around the second day. The timeline lasts anywhere from a few days to several weeks, with some individuals experiencing prolonged symptoms known as protracted withdrawal. Medical supervision is recommended for safe management during Xanax withdrawal, as abrupt cessation leads to life-threatening complications, including seizures.
The withdrawal timeline phases are as follows:
- Phase 1: Acute Withdrawal (First 24-48 hours): Symptoms like anxiety, irritability, and insomnia usually begin within hours of stopping Xanax, with peak intensity around the second day. Physical symptoms such as tremors, sweating, and headaches are common during this phase.
- Phase 2: Peak Withdrawal (Days 2-5): This is the most intense period, with symptoms like anxiety, difficulty concentrating, and mood swings reaching their peak. Individuals also experience more severe symptoms, such as confusion or agitation.
- Phase 3: Subacute Withdrawal (Days 5-14): As symptoms start to subside, individuals still experience residual effects, including insomnia, low energy, and anxiety. These symptoms gradually improve but persist for up to two weeks.
- Phase 4: Protracted Withdrawal (Weeks to Months): In some cases, withdrawal symptoms extend beyond the acute phase, with lingering symptoms like depression, anxiety, and sleep disturbances. This extended period of withdrawal lasts anywhere from 1 to 4 weeks and is more common in those who have used Xanax for long periods or at high doses.
How to Help Someone with a Xanax Addiction?
To help someone with a Xanax addiction, it is important to approach the situation with empathy, patience, and understanding. Start by offering emotional support and encouraging them to seek professional help from a healthcare provider or addiction specialist. Express concern for their well-being without judgment, and let them know that they are not alone in their struggle. Addiction treatment methods such as cognitive-behavioral therapy (CBT) and medication-assisted treatment (MAT) are effective in managing Xanax dependence, and encouraging them to explore these options is a good first step.
Another important aspect is helping them create a support system, which includes involvement in support groups such as Narcotics Anonymous (NA) or local addiction recovery programs. These groups provide a sense of community and accountability, which are necessary in the recovery process. Additionally, it is important to encourage gradual tapering under medical supervision, as abrupt cessation leads to dangerous withdrawal symptoms. Helping them navigate these steps, offering encouragement, and staying involved in their recovery process significantly improve their chances of overcoming addiction.
How Does Xanax Addiction Relate to Co-Occurring Disorders?
Xanax addiction relates to co-occurring disorders because individuals who have an addiction have underlying mental health conditions, which have contributed to their substance use in the first place. Co-occurring disorders, such as anxiety, depression, and alcohol use disorder, frequently overlap with Xanax addiction. In fact, research by the National Institute on Drug Abuse shows that approximately 20-30% of people with substance use disorders also experience mental health conditions like anxiety or depression. Xanax, being a medication primarily used to treat anxiety and panic disorders, is misused by individuals as a form of self-medication for these co-occurring disorders, making the addiction more complex and difficult to treat.
For instance, individuals with anxiety disorders develop a dependency on Xanax as a way to alleviate their chronic stress or panic attacks. This, in turn, leads to increased use and eventual addiction. Similarly, people suffering from depression or other mood disorders use Xanax to cope with their symptoms, which escalate into misuse. Moreover, individuals with alcohol use disorder use Xanax alongside alcohol, increasing the risk of overdose and intensifying both physical and psychological dependence. Treating Xanax addiction effectively requires addressing these co-occurring mental health disorders simultaneously, a process known as integrated treatment, to ensure long-term recovery success.
Is Xanax a Benzodiazepine?
Yes, Xanax is a benzodiazepine. It belongs to a class of drugs known for their sedative and calming effects on the central nervous system. Benzodiazepines, including Xanax (alprazolam), work by enhancing the activity of gamma-aminobutyric acid (GABA), a neurotransmitter that inhibits brain activity, leading to relaxation, reduced anxiety, and muscle relaxation. Benzodiazepines are prescribed for anxiety, panic disorders, and other related conditions. However, they also carry a risk of dependence and addiction when used over extended periods or misused.
What’s the Difference Between Xanax vs Klonopin?
The main difference between Xanax and Klonopin is their duration of action. Xanax (alprazolam) has a short half-life, lasting 6-12 hours, making it effective for immediate relief of anxiety or panic attacks. It acts quickly, but its effects wear off relatively fast. In contrast, Klonopin (clonazepam) has a longer half-life, ranging from 18-50 hours, which means its effects last much longer and are used for longer-term management of anxiety and panic disorders, as studied by WebMD in “Clonazepam (Klonopin) – Uses, Side Effects, and More.”
Xanax is commonly prescribed for acute anxiety or panic attacks due to its fast onset, while Klonopin is used for generalized anxiety disorder (GAD) or as a seizure control medication. The longer-lasting effects of Klonopin are more suitable for people who need continuous anxiety management, whereas Xanax is prescribed for short-term use because of its potential for dependence and misuse. Both medications are benzodiazepines, meaning they share similar properties and risks, including the potential for addiction, but their use cases and duration of action differ significantly.
How Does Xanax Addiction Differ From Alcohol Addiction?
Xanax addiction differs from alcohol addiction primarily in its mechanisms of action, effects, and withdrawal processes. Xanax, a benzodiazepine, works by enhancing the inhibitory effects of GABA in the brain, leading to calming, anxiolytic effects. It is prescribed for short-term use to treat anxiety and panic disorders, but misuse quickly leads to dependence and addiction. Alcohol, on the other hand, is a central nervous system depressant that also enhances GABA activity but through different pathways, and it causes physical and psychological dependence over time with chronic use.
While both substances cause dependence and withdrawal symptoms, the specifics vary. Xanax withdrawal includes severe anxiety, particularly if the drug is stopped abruptly, according to Healthline. Alcohol withdrawal, while also severe in cases of prolonged use, is more commonly associated with delirium tremens (DTs), which include tremors, hallucinations, and life-threatening cardiovascular instability. The treatment for both conditions involves gradual tapering under medical supervision, but the approach differs based on the substance’s pharmacokinetics and the severity of the addiction.
The social and behavioral contexts of addiction differ—alcohol consumption is more socially accepted in many cultures, making alcohol addiction more visible, whereas Xanax addiction is less noticeable in the early stages since it involves prescription misuse. Both addictions co-occur with mental health disorders, like depression or anxiety, but Xanax addiction is especially linked to anxiety disorders, while alcohol dependence is more closely associated with social and environmental factors.
How Does Xanax Addiction Differ From Valium Addiction?
Xanax addiction differs from Valium addiction primarily in its chemical composition, potency, and the duration of its effects. Xanax (alprazolam) is a short-acting benzodiazepine, while Valium (diazepam) is a long-acting benzodiazepine. This difference in how long the drugs stay in the system affects both their potential for abuse and the severity of withdrawal symptoms. Xanax has a faster onset and a more intense effect, which makes it more prone to misuse, while Valium’s slower onset and longer half-life make it less likely to be abused in the same manner.
In terms of addiction, Xanax is associated with the quick development of dependence due to its rapid onset and short duration of action. Users take more frequent doses to maintain the drug’s calming effects, increasing the potential for misuse and addiction. Valium, on the other hand, is less likely to cause immediate dependence, but misuse over time still leads to addiction, particularly due to its long half-life, which allows it to accumulate in the body. Withdrawal from Xanax is more intense and acute, with symptoms such as anxiety and agitation, while Valium withdrawal is less severe due to its gradual elimination from the body. However, both Xanax and Valium cause severe withdrawal symptoms, including seizures, if not properly tapered under medical supervision.
Both drugs are used to treat anxiety, muscle spasms, and other conditions, but due to the differences in their pharmacokinetics, the addiction profiles and treatment approaches for Xanax and Valium differ significantly. While both drugs carry risks of addiction and overdose, Xanax has a higher potential for abuse and dependence, according to Healthline.
Valium misuse rates show that 1.4% of the U.S. population, or about 3.9 million people, report misusing benzodiazepines like Valium annually, according to Addiction Help. Women are more likely to be prescribed Valium, and they experience stronger cravings compared to men. Misuse is more common among younger adults (18-35), while older adults (65 and above) have higher prescribed use of Valium and Xanax both.
Find Drug Rehabilitation Centers Near You Anywhere In the US
Addiction Resource team has compiled an extensive list of the top drug rehabilitation facilities around the country. Use our locator tool to find the best centers near you.



 FindTreatment.gov
FindTreatment.gov